Scientific perspectives on Guillain-Barre Syndrome (GBS): A comprehensive review for sentience after early 2025 GBS outbreak in an Indian state
DOI:
https://doi.org/10.69857/joapr.v13i4.1091Keywords:
Guillain-Barré Syndrome (GBS), Pathophysiology, Risk factors, Diagnosis, Treatment options, Current research advancesAbstract
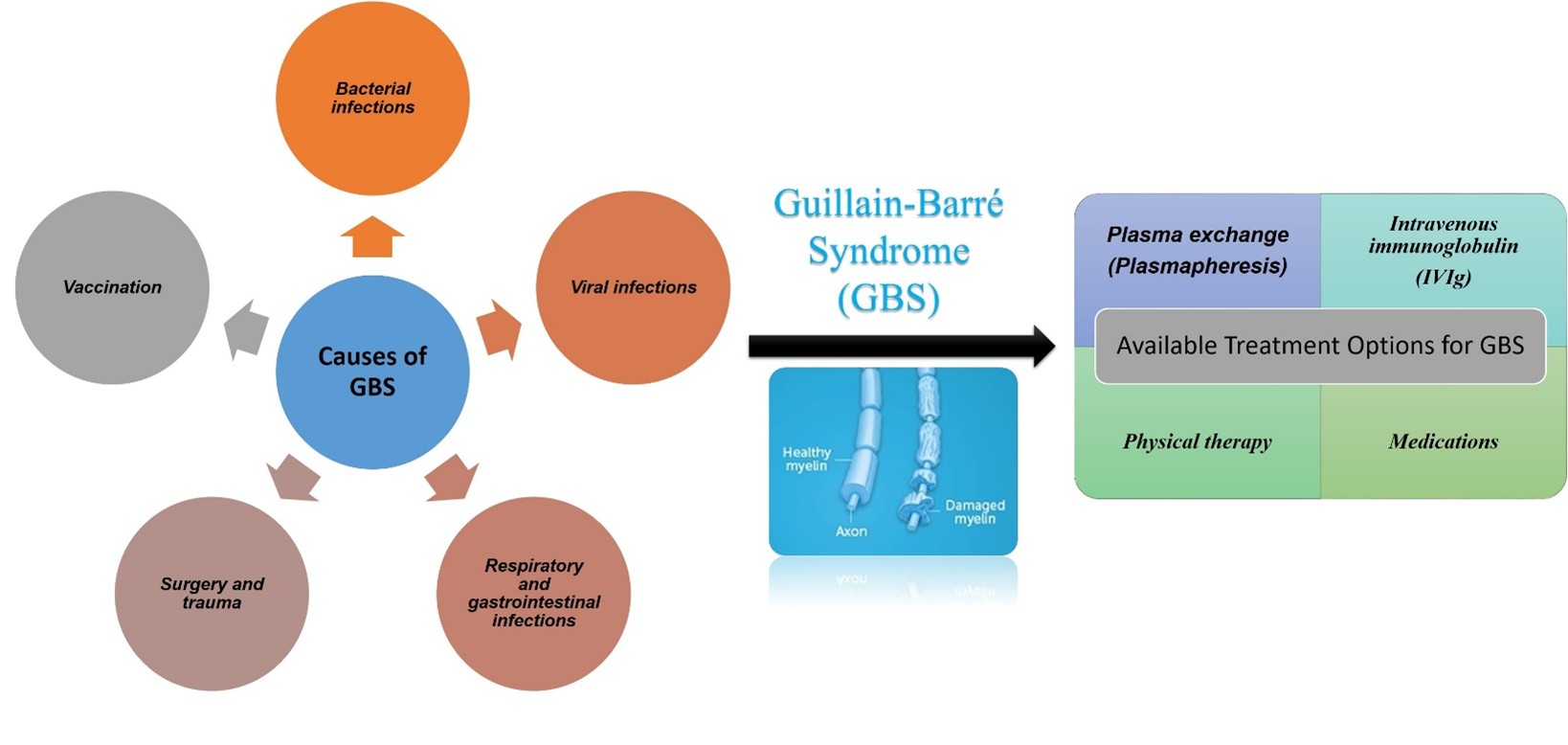
Background: Guillain-Barré Syndrome (GBS) is an acute, self-limiting, and rare neurological disorder wherein the body's immune system mistakenly attacks the peripheral nervous system (PNS). A report, published in February 2025 by the Indian newspaper ‘The Times of India’, highlighted a significant outbreak of GBS in the Indian state of Maharashtra, owing to the Campylobacter jejuni (C. jejuni) infection. The surge in cases has been considered as one of the most significant recorded GBS outbreaks globally, which underscores the need to raise GBS awareness. Method: This article provides an in-depth scientific perspective on GBS, drawing on literature from scientific databases such as PubMed and ScienceDirect. It aims to enhance awareness among science-related students, researchers, medical and paramedical professionals, and the general public. Result and discussion: GBS is an acute polyneuropathy characterized by limb weakness with hyporeflexia or areflexia. In severe forms, respiratory and bulbar paralysis can occur, requiring mechanical ventilatory support. It is the commonest cause of acute neuromuscular paralysis. The basic underlying mechanism of the disease is a localized attack against the myelin sheath of the peripheral nerves and nerve roots, with secondary axonal damage. It is believed that the bacterial antigens have a close molecular mimicry with neural antigens. As a result, the response generated against these antigens cross-reacts with the neural cells. Plasma exchange, immunoglobulin infusion, and plasmapheresis are the mainstays of treatment for GBS. Conclusion: A thorough understanding of GBS is essential, including its pathophysiology, underlying causes, risk factors, symptoms, diagnostic methods, treatment strategies, and the latest advancements.
Downloads
References
Hosseininezhad M, Khatami SS, Saadat S, Asghari M, Ghovvati Choshal H, Hooshmand Marvasti A, Gholipour Soleimani Z. Ten years evaluation of epidemiology- and mortality-related factors in adults and children with Guillain-Barré syndrome in the north of Iran. Neurol. Sci., 43, 1929-1938 (2022) https://doi.org/10.1007/s10072-021-05562-y.
Luo HY, Li XJ, Cheng M, Wang J, Xie L, Yao Z, Jiang. Clinical characteristics of children with Guillain-Barré syndrome and factors associated with disease severity. J Clin Neurosci., 92, 120-125 (2021) https://doi.org/10.1016/j.jocn.2021.08.001.
Dang HH, Nguyen HLT. Comparison of clinical features, short-term outcome of Guillain-Barré syndrome between adults and children: a retrospective study in Vietnam. Pediatr Neurol., 155, 177-181 (2024) https://doi.org/10.1016/j.pediatrneurol.2024.03.034.
Zheng P, Tian DC, Xiu Y, Wang Y, Shi FD. Incidence of Guillain-Barré syndrome (GBS) in China: a national population-based study. Lancet Reg Health West Pac., 18, 100302 (2021) https://doi.org/10.1016/j.lanwpc.2021.100302
Singh A, Jain E, Sharma V, Sinha A, Khaliq W. Guillain-Barré syndrome presenting as painful weakness and edema of the legs: A case report. Cureus., 15(6), e40641 (2023) https://doi.org/10.7759/cureus.40641.
Li Q, Liu J, Jiang W, Jiang L, Lu M, Xiao L, Li Y, Lan Y. A case of brucellosis-induced Guillain–Barré syndrome. BMC Infect Dis., 22(1), 72 (2022) https://doi.org/10.1186/s12879-021-07025-3.
Wachira VK, Farinasso CM, Silva RB, Peixoto HM, de Oliveira MRF. Incidence of Guillain-Barré syndrome in the world between 1985 and 2020: A systematic review. Glob Epidemiol., 5, 100098 (2023) https://doi.org/10.1016/j.gloepi.2023.100098.
Papri N, Islam Z, Leonhard SE, Mohammad Q, Endtz H, Jacobs B. Guillain–Barré syndrome in low-income and middle-income countries: challenges and prospects. Nat Rev Neurol., 17(5), 285-296 (2021) 10.1038/s41582-021-00467-y.
Van Doorn PA, van den Bergh PY, Hadden RD, Avau B, Venkurnkelsvn P, Attarian S, Markens PH, Cornblath D, Goedee H, Jacobs D, Lunn M, Qurerol L, Rajabelly Y, Umapathi T, Toplaglu H, Willison H. European Academy of Neurology/Peripheral Nerve Society guideline on diagnosis and treatment of Guillain–Barré syndrome. J Peripher Nerv Syst., 30(12), 3646-3674 (2023) https://doi.org/10.1111/jns.12594.
Khan SA, Das PR, Nahar Z, Dewan SMR. An updated review on Guillain-Barré syndrome: challenges in infection prevention and control in low- and middle-income countries. SAGE Open Med., 12, 20503121241239538 (2024) https://doi.org/10.1177/20503121241239538.
Koike H, Chiba A, Katsuno M. Emerging infection, vaccination, and Guillain–Barré syndrome: a review. Neurol Ther., 10(2), 523-537 (2021) https://doi.org/10.1007/s40120-021-00261-4.
Rostami F, Tahernia H, Noorbakhsh M. Diagnosis and treatment of Guillain-Barre syndrome and neurological problems with a clinical approach: a systematic review. J Pharm Negative Results., 4094-4111 (2022) https://doi.org/10.47750/pnr.2022.13.S10.496.
Hagen KM, Ousman SS. The neuroimmunology of Guillain-Barré syndrome and the potential role of an aging immune system. Front Aging Neurosci., 13, 613628 (2021) https://doi.org/10.3389/fnagi.2020.613628
Yadav N, Pragati, Dwivedi MK. Microorganisms in pathogenesis and management of Guillain–Barré syndrome (GBS). In: Role of Microorganisms in Pathogenesis and Management of Autoimmune Diseases: Volume II: Kidney, Central Nervous System, Eye, Blood, Blood Vessels & Bowel. Singapore: Springer Nature Singapore; 12(8), 177-194 (2023) https://doi.org/10.1007/978-981-19-4800-8_9
Shastri A, Al Aiyan A, Kishore U, Farrugia ME. Immune-mediated neuropathies: pathophysiology and management. Int J Mol Sci., 24(8), 7288 (2023) https://doi.org/10.3390/ijms24087288.
Chabchoub I, Snoussi M, Ammar R, Salah R, Dhammak C, Frikha F, Bouaziz M, Boudwara T, Bahoul Z. About a rare association: Guillain–Barré syndrome and polymyositis. Clin Case Rep., 10(11), e6642 (2022) https://doi.org/10.3390/ijms24087288.
Ngarka L, Siewe Fodjo JN, Aly E, Masocha W, Njamnshi AK. The interplay between neuroinfections, the immune system and neurological disorders: a focus on Africa. Front Immunol., 12, 803475 (2022) https://doi.org/10.3389/fimmu.2021.803475.
Mominur Rahman M, Afsana Mim S, Afroza Alam Tumpa M, Taslim Sarker M, Ahmed M, Alghamdi BS, Hafeez A, Alexiou A, Perveen A, Md Ashraf G. Exploring the management approaches of cytokines including viral infection and neuroinflammation for neurological disorders. Cytokine., 157, 155962 (2022) https://doi.org/10.1016/j.cyto.2022.155962.
Passaro AP, Lebos AL, Yao Y, Stice SL. Immune response in neurological pathology: emerging role of central and peripheral immune crosstalk. Front Immunol., 12, 676621 (2021) https://doi.org/10.3389/fimmu.2021.676621.
Berciano J. Pathophysiology and markers of very early classic Guillain-Barré syndrome. NeuroMarkers., 1(1), 10003 (2024) https://doi.org/10.1016/j.neumar.2024.100003.
Berciano J. Axonal pathology in early stages of Guillain-Barré syndrome. Neurol., 37(6), 466-479 (2022) https://doi.org/10.1016/j.nrleng.2020.08.001.
Berciano J. Microscopical anatomy of the peripheral nervous system: an essential notion for understanding the pathophysiology of very early classic Guillain‐Barré syndrome. Neuropathology., 45(2), 85-99 (2024) https://doi.org/10.1111/neup.13006.
Malekpour M, Khanmohammadi S, Meybodi MJE, Shekpouh D, Rahmanian M, Kardeh S, Azarpira N. COVID‐19 as a trigger of Guillain‐Barré syndrome: a review of the molecular mechanism. Immun Inflamm Dis., 11(5), e875 (2023) https://doi.org/10.1002/iid3.875
Itahashi K, Irie T, Nishikawa H. Regulatory T‐cell development in the tumor microenvironment. Eur J Immunol., 52(8), 1216-1227 (2022) https://doi.org/10.1002/eji.202149358
Reynolds CA, Pelka S, Gjergjova F, Tasset I, Khawaja R, Cuervo A. Restoration of LAMP2A expression in old mice leads to changes in the T cell compartment that support improved immune function. Proc Natl Acad Sci USA., 121(38), e2322929121 (2024) https://doi.org/10.1073/pnas.2322929121.
Merkenschlager J, Berz RM, Ramos V, Uhlig M, MacLean A, Nowosad C, Oliviera T, Nussenzweig M. Continually recruited naïve T cells contribute to the follicular helper and regulatory T cell pools in germinal centers. Nat Commun., 14(1), 6944 (2023) https://doi.org/10.1038/s41467-023-41880-9.
Jairaman A, Othy S, Dynes JL, Pathak M, Cahalan S. Piezo1 channels restrain regulatory T cells but are dispensable for effector CD4+ T cell responses. Sci Adv., 7(7), eabg5859 (2021) https://doi.org/10.1126/sciadv.abg5859.
Krovi SH, Kuchroo VK. Activation pathways that drive CD4+ T cells to break tolerance in autoimmune diseases. Immunol Rev., 307(1), 161-190 (2022) https://doi.org/10.1111/imr.13071.
Zhao Y, Zhang Q, Zhang B, Dai Y, Gao Y, Li C, Yu Y, Li C. Epstein–Barr viruses: their immune evasion strategies and implications for autoimmune diseases. Int J Mol Sci., 25(15), 8160 (2024) https://doi.org/10.3390/ijms25158160.
Seliger B, Massa C. Immune therapy resistance and immune escape of tumors. Cancers., 13(3), 551 (2021) https://doi.org/10.3390/cancers13030551.
Li KJ, Wu CH, Lu CH, Yu Ll. Trogocytosis between non-immune cells for cell clearance, and among immune-related cells for modulating immune responses and autoimmunity. Int J Mol Sci., 22(5), 2236 (2021) https://doi.org/10.3390/ijms22052236.
Rothlin CV, Hille TD, Ghosh S. Determining the effector response to cell death. Nat Rev Immunol., 21(5), 292-304 (2021) https://doi.org/10.1038/s41577-020-00456-0.
Velardi E, Tsai JJ, van den Brink MRM. T cell regeneration after immunological injury. Nat Rev Immunol., 21, 277–291 (2021) https://doi.org/10.1038/s41577-020-00457-z.
Jarjour NN, Masopust D, Jameson SC. T cell memory: understanding COVID-19. Immunity., 54(1), 14-18 (2021) https://doi.org/10.1016/j.immuni.2020.12.009.
Bragazzi NL, Kolahi AA, Nejadghaderi SA, Lochner P, Brigo F, Naldi A, Lanteri P, Garbarino S, Sullman MJM, Dai H, Wu J, Kong JD, Jahrami H, Sohrabi MR, Safiri S. Global, regional, and national burden of Guillain-Barré syndrome and its underlying causes from 1990 to 2019. J Neuroinflammation., 18(1), 264 (2021) https://doi.org/10.1038/s41582-021-00467-y.
Singh J, Kumar N, Dinkar A. Demographic, clinical, and investigational characteristics of COVID-19-related Guillain-Barré syndrome with differences from typical and another virus-related Guillain-Barré syndrome. Infect Dis Drug Targets., 22(7), 27-38 (2022) https://doi.org/10.2174/1871526522666220429134113.
Aragonès JM, Altimiras J, Alonso F, Celedón G, Alfonso S, Roura P, Moreira A. Incidence and clinical characteristics of Guillain-Barré syndrome in Osona (Barcelona, Spain), 2003-2016. Neurol (Engl Ed)., 36(7), 525-530 (2021) https://doi.org/10.1016/j.nrleng.2018.03.020.
Suci YD, Rosyid AN, Wulaa NL, Alamsyah M, Irmayani Ak, Bachrun T. Guillain-Barré syndrome and multiple lacunar infarcts in a COVID-19 patient. J Infect Dev Ctries., 17(11), 1641-1646 (2023) https://doi.org/10.3855/jidc.17975.
Abdallah EM, Sulieman AME. New discoveries in toxins from Campylobacter. In: Microbial Toxins in Food Systems: Causes, Mechanisms, Complications, and Metabolism. Cham: Springer Nature Switzerland; 319-331 (2024) https://doi.org/10.1007/978-3-031-62839-9_24.
Clarke AK, Ajlouni S. Recommended practices to eliminate Campylobacter from live birds and chicken meat in Japan. Food Safety., 9(3), 57–74 (2021) https://doi.org/10.14252/foodsafetyfscj.D-20-00021.
Quino W, Caro-Castro J, Mestanza O, Hurtado V, Zamudio ML, Cruz-Gonzales G, Gavilan RG. Emergence and molecular epidemiology of Campylobacter jejuni ST-2993 associated with a large outbreak of Guillain-Barré syndrome in Peru. Microbiol Spectrum., 10(5), e01187-22 (2022) https://doi.org/10.1128/spectrum.01187-22.
Heikema AP, Strepis N, Horst-Kreft D, Huynh S, Zomer A, Kelly DJ, Cooper KK, Parker CT. Biomolecule sulphation and novel methylations related to Guillain-Barré syndrome-associated Campylobacter jejuni serotype HS:19. Microb Genom., 7, 000660 (2021) https://doi.org/10.1099/mgen.0.000660.
Imbrea AM, Balta I, Dumitrescu G, McCleery D, Pet I, Iancu T, Stef L, Corcionivoschi N, Liliana PC. Exploring the contribution of Campylobacter jejuni to post-infectious irritable bowel syndrome: a literature review. Appl Sci., 14, 3373 (2024) https://doi.org/10.3390/app14083373.
Lopes GV, Ramires T, Kleinubing NR, Scheik LK, Fiorentini AM, Silva W. Virulence factors of foodborne pathogen Campylobacter jejuni. Microb Pathog., 161, 105265 (2021) https://doi.org/10.1016/j.micpath.2021.105265.
Panzenhagen P, Portes AB, Dos Santos AM, Duque SDS, Conte Junior CA. The distribution of Campylobacter jejuni virulence genes in genomes worldwide derived from the NCBI pathogen detection database. Genes., 12, 1538 (2021) https://doi.org/10.3390/genes12101538.
Gabbert AD, Mydosh JL, Talukdar PK, Gloss LM, McDermott JE, Cooper KK, Clair GC, Konkel ME. The missing pieces: the role of secretion systems in Campylobacter jejuni virulence. Biomolecules., 13, 135 (2023) https://doi.org/10.3390/genes12101538.
Li XV, Leonardi I, Putzel GG, Semon A, Fiers WD, Kusakabe T, Lin WY, Gao IH, Doron I, Gutierrez-Guerrero A, DeCelie MB, Carriche GM, Mesko M, Yang C, Naglik JR, Hube B, Scherl EJ, Iliev ID. Immune regulation by fungal strain diversity in inflammatory bowel disease. Nature., 603, 672-678 (2022) https://doi.org/10.1038/s41586-022-04502-w.
Mohammedsaleh ZM. The use of patient-specific stem cells in different autoimmune diseases. Saudi J Biol Sci., 29, 3338-3346 (2022) https://doi.org/10.1016/j.sjbs.2022.02.009.
Thapa D, Kumar V, Naik B, Kumar V, Gupta AK. Harnessing probiotic foods: managing cancer through gut health. Food Sci., 33, 2141-2160 (2024) https://doi.org/10.1007/s10068-024-01638-5.
Mayorgas A, Dotti I, Salas A. Microbial metabolites, postbiotics, and intestinal epithelial function. Mol Nutr Food Res., 65, 2000188 (2021) https://doi.org/10.1002/mnfr.202000188.
Łoniewski I, Banasiewicz T, Sieńko J, Skonieczna-Zydecka K, Stachowska E. Microbiota modifications in prehabilitation–the next step towards comprehensive preparation for surgery: the scoping review. Gastroenterol Rev., 19, 347-361 (2024) https://doi.org/10.5114/pg.2024.145833.
Özkan A, LoGrande NT, Feitor JF, Goyal G, Ingber G. Intestinal organ chips for disease modelling and personalized medicine. Nat Rev Gastroenterol Hepatol., 21, 751-773 (2024) https://doi.org/10.1038/s41575-024-00968-3.
Chakraborty U, Hati A, Chandra A. Covid-19 associated Guillain-Barré syndrome: a series of a relatively uncommon neurological complication. Diabetes Metab Syndr Clin Res Rev., 15, 102326 (2021) https://doi.org/10.1016/j.dsx.2021.102326.
Vega-Fernández JA, Suclupe-Campos DO, Coico-Vega MM, Aguilar-Gamboa FR. Viral etiology associated with Guillain-Barré syndrome: seeking an answer to the idiopathic. Rev Fac Med Humana., 22, 16 (2022) https://doi.org/10.1111/ene.16365.
Elendu C, Osamuyi EI, Afolayan IA, Opara N, Anunaso C, Petrson J. Clinical presentation and symptomatology of Guillain-Barré syndrome: a literature review. Medicine., 103, e38890 (2024) https://doi.org/10.1097/MD.0000000000038890.
Luijten LW, Leonhard SE, van der Eijk AA, Doets A, Briani A, Garresen M, Walgaard C, Tsouni P, Vicino A, Visser L, Ripellino P, Jacobs B. Guillain-Barré syndrome after SARS-CoV-2 infection in an international prospective cohort study. Brain., 144, 3392-3404 (2021) https://doi.org/10.1093/brain/awab279.
Bonilla C, Alvarez-Olmos MI, Uribe C, Fernández-Sarmiento J. Severe bradycardia in a teenager as the initial manifestation for Guillain-Barré syndrome: a case report. BMC Pediatr., 22, 152 (2022) https://doi.org/10.1186/s12887-022-03165-w.
Zhang Y, Huang C, Lu W, Hu Q. Case report: delayed Guillain-Barré syndrome following trauma: a case series and management considerations. Front Surg., 9, 903334 (2022) https://doi.org/10.3389/fsurg.2022.903334.
Gong Q, Liu S, Liu Y, Yao J, Fu X, Xiao Z, Lu Z. Guillain-Barré syndrome triggered by surgery in a Chinese population: a multicenter retrospective study. BMC Neurol., 21, 24647 (2021) https://doi.org/10.1186/s12883-021-02067-1.
Abwini LZ, Rana D, Crincoli J, Bowden FG, McAlpin F. Recurrent Guillain-Barré syndrome after subsequent total knee arthroplasties. Arthroplast Today., 30, 101518 (2024) https://doi.org/10.1016/j.artd.2024.101518.
Tu WC, Chang ST, Huang CH, Cheng YY, Hsu CS. Guillain-Barré syndrome with respiratory failure following spine surgery for incomplete cervical cord injury: a case report and literature review. Medicina., 58, 1063 (2022) https://doi.org/10.3390/medicina58081063.
Wang F, Wang D, Wang Y, Wang W, Wang Y, Hou H. Population-based incidence of Guillain-Barré syndrome during mass immunization with viral vaccines: a pooled analysis. Front Immunol., 13, 782198 (2022) https://doi.org/10.3389/fimmu.2022.782198.
Jeong YD, Park S, Lee S, Jang W, Rahmati M, Lee H, Yon D. Global burden of vaccine-associated Guillain-Barré syndrome over 170 countries from 1967 to 2023. Sci Rep., 14(1), 24561 (2024) https://doi.org/10.1038/s41598-024-74729-2.
Huang Y, Luo C, Jiang Y, Du J, Tao C, Hao Y. A Bayesian network to predict the risk of post influenza vaccination Guillain-Barré syndrome: Development and validation study. JMIR Public Health Surveill., 8(3), e25658 (2022) https://doi.org/10.2196/25658.
Walters J. Weakness in the intensive care unit. Pract Neurol., 21, 2022-003422 (2022) https://doi.org/10.1136/pn-2022-003422.
Doneddu PE, Pensato U, Iorfida A, Alberti C. Neuropathic pain in the emergency setting: Diagnosis and management. J Clin Med., 12(18), 6028 (2023) https://doi.org/10.3390/jcm12186028.
Racke MK, Frohman EM, Frohman T. Pain in multiple sclerosis: Understanding pathophysiology, diagnosis, and management through clinical vignettes. Front Neurol., 13, 799698 (2022) https://doi.org/10.3389/fneur.2021.799698.
Olander A, Andersson H, Sundler AJ, Hagiwara MA, Bremer A. The onset of sepsis as experienced by patients and family members: A qualitative interview study. J Clin Nurs., 32(19-20), 7402-7411 (2023) https://doi.org/10.1111/jocn.16785.
Asghari E, Gholizadeh L, Kazami L, Sadeghi M, Saparham M, Agdam N. Symptom recognition and treatment-seeking behaviors in women experiencing acute coronary syndrome for the first time: A qualitative study. BMC Cardiovasc Disord., 22(1), 508 (2022) https://doi.org/10.1186/s12872-022-02892-3.
Yaamika H, Muralidas D, Elumalai K. Review of adverse events associated with COVID-19 vaccines, highlighting their frequencies and reported cases. J Taibah Univ Med Sci., 18, 619-629 (2023) https://doi.org/10.1016/j.jtumed.2023.08.004.
Bakke I, Lund CG, Carlsson M, Salvesen R, Normann B. Barriers to and facilitators for making emergency calls–a qualitative interview study of stroke patients and witnesses. J Stroke Cerebrovasc Dis., 31(10), 106734 (2022) https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106734.
Th’ng F, Rao KA, Huang PY. Case series: Acupuncture-related pneumothorax. Int J Emerg Med., 15(1), 48 (2022) https://doi.org/10.1186/s12245-022-00455-z.
Koike H, Katsuno M. Emerging infectious diseases, vaccines and Guillain–Barré syndrome. Clin Exp Neuroimmunol., 12(3), 165-170 (2021) https://doi.org/10.1111/cen3.12644.
Aguilar-Parra LG, Rodríguez-Jiménez KV, Saráchaga AJD, Jiménez EM, Olalde J, Rotenberg N, Hernández J. Frequency, clinical, and paraclinical characteristics of patients with Bickerstaff brainstem encephalitis in a tertiary-referral neurological center. Rev Mex Neurosci., 23(2), 57-62 (2022) https://doi.org/10.24875/rmn.21000050.
Nerella N, Vasudha B. Design, development, and optimization of sumatriptan loaded ethosomal intra-nasal nanogel for brain targeting. J. Appl. Pharm. Res., 12, 83–98 (2024) https://doi.org/10.69857/joapr.v12i4.610.
Handzic A, Margolin E. Bickerstaff brainstem encephalitis with exceptionally fast recovery. J Neuro-Ophthalmol., 42(1), 65-67 (2022) https://doi.org/10.1097/WNO.0000000000002200.
Wang H. A case of Miller Fisher syndrome overlapped by Bickerstaff's brainstem encephalitis and Guillain-Barré syndrome. Ann Clin Med Case Rep., 10, 1596850 (2024) https://doi.org/10.1155/2016/1596850.
Wagle L, Reyes A, Regmi R, Regmi DR, Thapa A. Multiple cranial nerve palsies without limb weakness: A rare cranial variant of Guillain-Barré syndrome. Cureus., 16(5), e60013 (2024) https://doi.org/10.7759/cureus.60013.
Andalib S, Biller J, Di Napoli M, Moghimi N, Nobleza C, Camejo C, Diveni A. Peripheral nervous system manifestations associated with COVID-19. Curr Neurol Neurosci Rep., 21, 14 (2021) https://doi.org/10.1007/s11910-021-01102-5.
Damjan H. Kranialni polinevritis, povezan z okužbo s SARS-CoV-2: prikaz primera. Polyneuritis cranialis related to SARS-CoV-2 infection: a case report. Academia.edu., 16(1), 53-56 (2023) https://doi.org/10.18690/actabiomed.251.
Duggal AK. Guillain-Barré syndrome and its variants. J Indian Acad Clin Med., 19(4), 278-291 (2018) https://doi.org/10.1016/j.ncl.2013.01.005.
Noioso C, Bevilacqua L, Barone P. Miller Fisher Syndrome: What it is, symptoms & treatment. Clin Case Rep Int., 14, 1250774 (2023) https://doi.org/10.3389/fneur.2023.1250774.
Zhao F, Wang J, Zhang J, Pang X, Huang S, Zang W. Pain in acute motor axonal neuropathy. Muscle Nerve., 64(6), 739-743 (2021) https://doi.org/10.1002/mus.27414.
Shang P, Zhu M, Wang Y, Laudanski K. Pain in Guillain-Barré syndrome: A retrospective study of clinical characteristics and prognostic factors. J Neurol., 268(7), 2402-2419 (2021) https://doi.org/10.1186/s12883-025-04061-3.
Nakamura Y, Motoki M, Hirose T, Ishida S, Arawaka S. Fulminant Guillain-Barré syndrome showing severe pharyngeal-cervical-brachial weakness in the recovery phase: A case report. BMC Neurol., 19, 145 (2019) https://doi.org/10.1186/s12883-019-1376-5.
Ramos AP, Leonhard SE, Halstead SK, Meza R, Cornblath D, Umeres H, Pardo C. Guillain-Barré syndrome outbreak in Peru 2019 associated with Campylobacter jejuni infection. Neurol Neuroimmunol Neuroinflamm., 8(2), e952 (2021) https://doi.org/10.1212/NXI.0000000000000952.
Lupu VV, Miron I, Cianga AL, Gavrilovici C, Grigore I, David AG, Pertea LI, Grigore E, David DE, Lupu A. Diagnostic pitfalls in Guillain–Barré syndrome: Case report and literature review. Children., 9(12), 1969 (2022) https://doi.org/10.3390/children9121969.
Busl KM, Fried H, Muehlschlegel S, Madzar D, Varelas P, Waistermaier T, Weimer C. Guidelines for neuroprognostication in adults with Guillain–Barré syndrome. Neurocrit Care., 38(3), 564-583 (2023) https://doi.org/10.1007/s12028-023-01707-3.
Guémy C, Durand MC, Brisset M, Nicolas G. Changes in electrophysiological findings suggestive of demyelination following Guillain‐Barré syndrome: A retrospective study. Muscle Nerve., 68(6), 1467-1475 (2023) https://doi.org/10.1002/mus.27803.
Papri N, Islam Z, Ara G, Jacobs C, Mohammad Q. Management of Guillain–Barré syndrome in Bangladesh: Clinical practice, limitations and recommendations for low‐ and middle‐income countries. J Peripher Nerv Syst., 28(4), 564-577 (2023) https://doi.org/10.1111/jns.12597.
Kalita J, Kumar M, Misra UK. Prognostic significance of serial nerve conduction in GB syndrome. Neurol India., 70(5), 1995-2022 (2022) https://doi.org/10.4103/0028-3886.359245.
Rath J, Schober B, Zulehner G, Grisold A, Cetin H, Zimprich F. Nerve conduction studies in Guillain-Barré syndrome: Influence of timing and value of repeated measurements. J Neurol Sci., 420, 117267 (2021) https://doi.org/10.1016/j.jns.2020.117267.
Prashanth A, Shende V, Pawar S. A study of sensory nerve conduction in pre- and post-immunoglobulin treatment of Guillain-Barré syndrome. Cureus., 16(1), e51673 (2024) https://doi.org/10.7759/cureus.51673.
Thongchuam Y, Sukphulloprat P, Kulkantrakorn K. Diagnostic criteria and serial nerve conduction study for Guillain-Barré syndrome subtype diagnosis. Sci Technol Asia., 27(1), 125-133 (2022) https://ph02.tci-thaijo.org/index.php/SciTechAsia/article/view/248057.
Karunarathna I, De Alvis K, Gunasena P, Jayawardana A. The role of intra-abdominal pressure monitoring in managing ACS. Research Gate., 2(12), 49921 (2024) https://doi.org/10.4103/jiaps.JIAPS_222_15.
Hajjar LA, Costa IBSDS, Rizk SI, Val F, Lopes MD, Filho R, Teboul J, Landoni G. Intensive care management of patients with COVID-19: A practical approach. Ann Intensive Care., 11, 17 (2021) https://doi.org/10.1186/s13613-021-00820-w.
Hochman JS, Anthopolos R, Reynolds HR, Mavromichalis S. Survival after invasive or conservative management of stable coronary disease. Circulation., 147(1), 8-19 (2023) https://doi.org/10.1161/CIRCULATIONAHA.122.06271.
Savarirayan R, Ireland P, Irving M, Thompson D, Tunkvel D, Powell S, Thomas S, Wright M, Yasui N, Fredwall S. International consensus statement on the diagnosis, multidisciplinary management and lifelong care of individuals with achondroplasia. Nat Rev Endocrinol., 18(3), 173-189 (2022) https://doi.org/10.1038/s41574-021-00595-x.
Duong V, Daniel MS, Ferreira ML, Hunter G, Writsch C, Wei N, Nicolson P. Measuring adherence to unsupervised, conservative treatment for knee osteoarthritis: A systematic review. Osteoarthritis Cartilage Open., 3(2), 100171 (2021) https://doi.org/10.1016/j.ocarto.2021.100171.
Ali T, Hkima Abou Fakher F, Alawir M, Allababidi A, Sheikh Hasan A. Management of severe pediatric Guillain-Barré syndrome in a low-income country: Efficacy and safety of therapeutic plasma exchange in pediatric patients: A retrospective study. BMC Pediatr., 24(1), 818 (2024) https://doi.org/10.1186/s12887-024-05298-6.
Zaki HA, Iftikhar H, Najam M, Masood M, Fayed E, Shaban E. Plasma exchange (PE) versus intravenous immunoglobulin (IVIG) for the treatment of Guillain-Barré syndrome (GBS) in patients with severe symptoms: A systematic review and meta-analysis. Eneurol Sci., 31, 100468 (2023) https://doi.org/10.1016/j.ensci.2023.100468.
Fateen T, Sultana N, Sarwar M, Saqlain N. Complications of therapeutic plasma exchange in pediatric patients: An experience at a tertiary care hospital. Pak J Med Sci., 39(4), 994 (2023) https://doi.org/10.12669/pjms.39.4.7002.
Ali T, Abou Fakher FH, Alawir M, Allababidi A, Hasan AS. Efficacy and safety of therapeutic plasma exchange in pediatric patients with Guillain-Barré syndrome: A retrospective study. Research Square., 13(2), 16323 (2024) https://doi.org/10.21203/rs.3.rs-3892021/v1.
Atay G, Demirkol D. Therapeutic plasma exchange application in children requires individual decision. J Pediatr Intensive Care., 10(2), 106-109 (2021) https://doi.org/10.1055/s-0040-1714098.
Bondi M, Engel-Haber E, Wolff J, Rimon L, Zeilig G. Functional outcomes following inpatient rehabilitation of Guillain-Barré syndrome patients: Intravenous immunoglobulins versus plasma exchange. Neurorehabilitation., 48(4), 543-551 (2021) https://doi.org/10.3233/NRE-201640.
Rajabally YA. Immunoglobulin and monoclonal antibody therapies in Guillain-Barré syndrome. Neurotherapeutics., 19(3), 885-896 (2022) https://doi.org/10.1007/s13311-022-01253-4.
Shrisunder N, Dhakad PK, Gilhotra R. Development of a Fast-Acting Nanosuspension Nasal Drop Using a Novel Co-Processed Polymer for Migraine Relief. J. Appl. Pharm. Res., 13, 164–78 (2025) https://doi.org/10.69857/joapr.v13i3.940.
Arun TC, Takoor S, Ramchandani S, Vijapurkar S, Sandeep G. Supraglottic airway device in a patient with Guillain-Barre syndrome undergoing lower-segment cesarean section (LSCS): A case report. Cureus., 17(1), e77263 (2025) https://doi.org/10.7759/cureus.77263.
Martinelli-Boneschi F, Colombo A, Bresolin N, Sessa M, Bassi P, Grampa G, et al. COVID-19-associated Guillain-Barré syndrome in the early pandemic experience in Lombardia (Italy). Neurol Sci., 44(2), 437-446 (2023) https://doi.org/10.1007/s10072-022-06429-6.
Chandran NP, Panthappulan H, Pradeep K. A scoping review on Guillain-Barré syndrome and its management—An Ayurvedic perspective. Kerala J Ayurveda., 3(4), 246-257 (2024) https://doi.org/10.55718/kja.332.
Pranay R, Tatikayala RK, Damera S, Pathakala N, Jadi RK. Insights of Nose To Brain Delivery in Treating Parkinson’S Disease: a Systematic Review. J. Appl. Pharm. Res., 12, 57–72 (2024) https://doi.org/10.69857/joapr.v12i6.625.
Cortinovis M, Perico N, Remuzzi G. Long-term follow-up of recovered patients with COVID-19. Lancet., 397(10270):173-175 (2021) https://doi.org/10.1016/S0140-6736(21)00039-8.
Horby PW, Pessoa-Amorim G, Peto L. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): Preliminary results of a randomised, controlled, open-label, platform trial. MedRxiv., 397(10285), 1637-1645 (2021) https://doi.org/10.1016/S0140-6736(21)00676-0.
Gupta S, Short SAP, Sise ME, Prosek JM, Madhavan SM, Soler MJ, et al. Acute kidney injury in patients treated with immune checkpoint inhibitors. J Immunother Cancer., 9(10), e003467 (2021) https://doi.org/10.1016/S0140-6736(21)00676-0.
Koshak AE, Koshak EA, Mobeireek AF, Badawi MA, Wali SO, Malibary HM, et al. Nigella sativa for the treatment of COVID-19: An open-label randomized controlled clinical trial. Complement Ther Med., 61,102769 (2021) https://doi.org/10.1016/j.ctim.2021.102769.
Li J, Xu D, Liu Y, He Z, Liao M. Acupuncture treatment of Guillain–Barré syndrome after using immune checkpoint inhibitors: A case report. Front Neurol., 13, 908282 (2022) https://doi.org/10.3389/fneur.2022.908282.
Rath J, Zulehner G, Schober B, Grisold A, Krenn M, Cetin H, Zimprich F. Real-world treatment of adult patients with Guillain-Barré syndrome over the last two decades. Sci Rep., 11(1),1-9 (2021) https://doi.org/10.1038/s41598-021-98501-y.
Gawande I, Akhuj A, Samal S. Effectiveness of physiotherapy intervention in Guillain Barre syndrome: A case report. Cureus., 16(1), e52062 (2024) https://doi.org/10.7759/cureus.52062.
Rajurkar R, Chavan N, Deodhe N, Baheti NC. Enhancing tone and strength in a patient with autoimmune encephalitis and Guillain-Barré syndrome using Rood's facilitatory techniques and neuromuscular electrical stimulation: A case report. Cureus., 16(3), e56054 (2024) https://doi.org/10.7759/cureus.56054.
Agnihotri S, Srivastava A, Gupta D, Naeem F. Rehabilitation of a chronic Guillain-Barré syndrome patient with vibratory motor stimulation of dorsiflexors: A case report. Cureus., 16(2), e53936 (2024) https://doi.org/10.7759/cureus.53936.
Kariya G, Salphale VG, Dadgal R. Effectiveness of symptomatic physiotherapy in enhancing the psychological parameters of a patient with Guillain-Barré syndrome: A case report. Cureus., 16(3), e55389 (2024) https://doi.org/10.7759/cureus.55389.
Russell G, Stapley S, Newlove-Delgado T, Salmon A, White R, Warren F, et al. Time trends in autism diagnosis over 20 years: A UK population‐based cohort study. J Child Psychol Psychiatry., 63(6), 674-682 (2022) https://doi.org/10.1111/jcpp.13505.
Dunstan DW, Dogra S, Carter SE, Owen N. Sit less and move more for cardiovascular health: Emerging insights and opportunities. Nat Rev Cardiol., 18(9), 637-648 (2021) https://doi.org/10.1038/s41569-021-00547-y.
Erdos J, Wild C. Mid- and long-term (at least 12 months) follow-up of patients with spinal muscular atrophy (SMA) treated with nusinersen, onasemnogene abeparvovec. Eur J Paediatr Neurol., 39, 1-10 (2022) https://doi.org/10.1016/j.ejpn.2022.04.006.
Walle-Hansen MM, Ranhoff AH, Mellingsæter M. Health-related quality of life, functional decline, and long-term mortality in older patients following hospitalisation due to COVID-19. BMC Geriatr., 21, 1-10 (2021) https://doi.org/10.1186/s12877-021-02140-x.
Vekaria B, Overton C, Wiśniowski A, Ahmad S, Aparicio-Castro A, Sebastain C, et al. Hospital length of stay for COVID-19 patients: Data-driven methods for forward planning. BMC Infect Dis., 21, 1-15 (2021) https://doi.org/10.1016/S0140-6736(24)00757-8.
Ardebili ME, Naserbakht M, Bernstein C, Hakimi H, Nodeeh F, Ranjbar R. Healthcare providers’ experience of working during the COVID-19 pandemic: A qualitative study. Am J Infect Control., 49(5), 547-554 (2021) https://doi.org/10.1016/j.ajic.2020.10.001.
Lorach H, Galvez A, Spagnolo V, Martel F, Karakas S, Intering N, et al. Walking naturally after spinal cord injury using a brain–spine interface. Nature., 618(7963), 126-133 (2023) https://doi.org/10.1038/s41586-023-06094-5.
Al Bayat S, Mundodan J, Hasnain S, Sallam M, Khogli, Ali D, et al. Can the cycle threshold (Ct) value of RT-PCR test for SARS-CoV-2 predict infectivity among close contacts? J Infect Public Health., 14(9), 1201-1205 (2021) https://doi.org/10.1016/j.jiph.2021.08.013.
Smith MP. Estimating total morbidity burden of COVID-19: Relative importance of death and disability. J Clin Epidemiol., 142, 54-59 (2022) https://doi.org/10.1016/j.jclinepi.2021.10.018.
Stiles MK, Wilde AA, Abrams DJ, Ackerman M, Albert C, Behr E, Chugh S, Cornel M, Gardner K, Ingles J, James C, Juang J, Kaab S, Kaufman E, Krahn A, Lubitz S, Macleod, Morrillo C, Nademanee K, Probst V, Saarel E, Sacilotto L, Semarian C, Shrppard M, Shimizu W, Skinner J, Hansen J, Wang D. APHR.S/HRS expert consensus statement on the investigation of decedents with sudden unexplained death and patients with sudden cardiac arrest, and of their families. Heart Rhythm., 18(1), e1-e50 (2021) https://doi.org/10.1016/j.hrthm.2020.10.010.
Sandroni C, Cronberg T, Sekhon M. Brain injury after cardiac arrest: Pathophysiology, treatment, and prognosis. Intensive Care Med., 47(12), 1393-1414 (2021) https://doi.org/10.1007/s00134-021-06548-2
Sharifian-Dorche M, Sahraian MA, Fadda G, Osherov, Dorsche A, Karaminia M, Saveriano A, Piana R, Antel J, Giacomini P. COVID-19 and disease-modifying therapies in patients with demyelinating diseases of the central nervous system: A systematic review. Mult Scler Relat Disord., 50, 102800 (2021) https://doi.org/10.1016/j.msard.2021.102800.
Pulatov SS. Efficacy of ipidacrine in the recovery period of ischaemic stroke. World Bull Public Health., 4(2), 4854 (2022).
Black RJ, Cross M, Haile LM. Global, regional, and national burden of rheumatoid arthritis, 1990–2020, and projections to 2050: A systematic analysis of the global burden of disease study 2021. Lancet Rheumatol., 5(10), e594-e610 (2023) https://doi.org/10.1016/S1474-4422(24)00038-3.
Tehrani S, Killander A, Åstrand P, Jakobsson J, Gille-Johnson P. Risk factors for death in adult COVID-19 patients: Frailty predicts fatal outcome in older patients. Int J Infect Dis., 102, 415-421 (2021) https://doi.org/10.1016/j.ijid.2020.10.071.
Kretch KS, Willett SL, Hsu LY, Sargent B, Harbourne R, Dusing S. Learn the Signs. Act Early.: Updates and implications for physical therapists. Pediatr Phys Ther., 34(4), 440-448 (2022) https://doi.org/10.1097/PEP.0000000000000937.
Serjeant S, Tighe B. A meta‐synthesis exploring caregiver experiences of home enteral tube feeding. J Hum Nutr Diet., 34(3),154754 (2022) https://doi.org/10.1111/jhn.12913.
Gradišnik P, Osterc Koprivšek A, Rus M, Golli T, Damjan H. Polyneuritis cranialis related to SARS-CoV-2 infection: a case report. Acta Medico-Biotechnica., 16(1), 53-56 (2023) https://doi.org/18690/actabiomed.251.
Kondziella D, Waldemar G. Clinical history and neuroanatomy: “Where is the lesion?”. Neurology at the Bedside. Neuro-Reactivation HV. Society of Neurology. Neurol Sci., 45(2), 4789 (2022).
Caputo F, Lungaro L, Galdi A, Zoli E, Giancola F, Caio G, De Giorgio R, Zoli G. Gastrointestinal Involvement in Anderson-Fabry Disease: A Narrative Review. Int J Environ Res Public Health., 18, 3320 (2021) https://doi.org/10.3390/ijerph18063320.
Jackson K, Parthan A, Lauher-Charest M, Broderick L, Law N, Barnett C. Understanding the symptom burden and impact of myasthenia gravis from the patient’s perspective: A qualitative study. Neurol Ther., 12(1),107-128 (2023) https://doi.org/10.1007/s40120-022-00408-x.
Laparidou D, Curtis F, Akanuwe J, Jackson J, Hodgson T, Siriwardena A. Patients’ experiences and perceptions of Guillain-Barré syndrome: A systematic review and meta-synthesis of qualitative research. PLoS One., 16(2), e0245826 (2021) https://doi.org/10.1371/journal.pone.0245826.
Biswas C. Work-related experience of adults after recovering from Guillain-Barré syndrome. CRP Bangladesh., 34(2), 2435363 (2023) https://doi.org/10.1080/09638280902822294.
Jackson J, Laparidou D, Siriwardena N. Exploring experiences of the illness, its care and recovery following Guillain-Barré syndrome-final report. Health Expect., 23(5),1338-1349 (2020) https://doi.org/10.1111/hex.13116
Shang P, Feng J, Wu W, Zhang HL. Intensive care and treatment of severe Guillain–Barré syndrome. Front Pharmacol., 12, 608130 (2021) https://doi.org/10.3389/fphar.2021.608130
Davidson I, Parker ZJ. Falls in people post‐Guillain‐Barré syndrome in the United Kingdom: A national cross‐sectional survey of community-based adults. Health Soc Care Community., 30(5), e2590-e2603 (2022) https://doi.org/10.1111/hsc.1370.
Harbo T, Andersen H. Neuromuscular effects and rehabilitation in Guillain-Barré syndrome. Zika Virus Impact., 2(4), 234-249 (2021) https://doi.org/10.1002/mus.26396.
Mayer JE, McNamara CA, Mayer J. Miller Fisher syndrome and Guillain-Barré syndrome: Dual intervention rehabilitation of a complex patient case. Physiother Theory Pract., 38(1), 245-254 (2022) https://doi.org/10.1080/09593985.2020.1736221.
Liu J, Tang F, Chen X, Li Z. Guillain-Barre syndrome with incomplete oculomotor nerve palsy after traumatic brain injury: Case report and literature review. Brain Sci., 13(4), 527 (2023) https://doi.org/10.3390/brainsci13040527.
Correll CU, Solmi M, Cortese S, Fava M, Hojlund M, Kraemer H, Mclyntr R, Pine D, Scheinder L, Kane J. The future of psychopharmacology: A critical appraisal of ongoing phase 2/3 trials, and of some current trends aiming to de‐risk trial programmes of novel agents. World Psychiatry., 22(1), 48-74 (2023) https://doi.org/10.1002/wps.21056.
Nwobodo D, Ugwu MC, Oliseloke Anie C, Al-Ouquili M, Ikem J, Chigozie U, Saki M. Antibiotic resistance: The challenges and some emerging strategies for tackling a global menace. J Clin Lab Anal., 36(9),e24655 (2022) https://doi.org/10.1002/jcla.24655.
Tabarsi P, Barati S, Jamaati H. Evaluating the effects of intravenous immunoglobulin (IVIg) on the management of severe COVID-19 cases: A randomized controlled trial. Int Immunopharmacol., 90,107205 (2021) https://doi.org/10.1016/j.intimp.2020.107205.
Mascellino MT, Di Timoteo F, De Angelis M, Oliva A. Overview of the main anti-SARS-CoV-2 vaccines: Mechanism of action, efficacy and safety. Infect Drug Resist., 14, 3459-3476 (2021) https://doi.org/10.2147/IDR.S315727.
Wojtukiewicz MZ, Rek MM, Karpowicz K, Gorska M, Politynska B, Wojtukiewicz A, Moniuszko M, Radiwon P, Tucker S, Honn K. Inhibitors of immune checkpoints—PD-1, PD-L1, CTLA-4—new opportunities for cancer patients and a new challenge for internists and general practitioners. Cancer Metastasis Rev., 40, 949-982 (2021) https://doi.org/10.1007/s10555-021-09976-0.
Zheng R, Zhang Y, Zhang K, Yuan Y, Jia S, Liu J. The complement system, aging, and aging-related diseases. Int J Mol Sci., 23(15), 8689 (2022) https://doi.org/10.3390/ijms23158689.
Armento A, Ueffing M, Clark SJ. The complement system in age-related macular degeneration. Cell Mol Life Sci., 78(10), 4487-4505 (2021) https://doi.org/10.1007/s00018-021-03796-9.
Ostrycharz E, Hukowska-Szematowicz B. New insights into the role of the complement system in human viral diseases. Biomolecules., 12(2), 226 (2022) https://doi.org/10.3390/biom12020226.
Querol LA, Hartung HP, Lewis RA, Doorn PA, Hammond T, Atassi N, Alonso-Alonso M, Dalaskas M. The role of the complement system in chronic inflammatory demyelinating polyneuropathy: Implications for complement-targeted therapies. Neurotherapeutics., 19(3), 864-873 (2022) https://doi.org/10.1007/s13311-022-01221-y.
Patry RT, Essler L, Andresen S, Quinn FD, Szymanski CM. Low-dose exposure to ganglioside-mimicking bacteria tolerizes human macrophages to Guillain-Barré syndrome-associated antigens. mBio., 13(1), e03852-21 (2022) https://doi.org/10.1128/mbio.03852-21.
Laman JD, Huizinga R, Boons GJ, Jacobs BC. Guillain-Barré syndrome: Expanding the concept of molecular mimicry. Trends Immunol., 43(4), 296-308 (2022) https://doi.org/10.1016/j.it.2022.02.003.
Shi P, Nian D, Qu H, Ye M, Wang C, Li L, Li QB. B. Infantis enhances immunotherapy for Guillain-Barre syndrome through regulating PD-1. BMC Neurol., 23(1), 3468 (2023) https://doi.org/10.1186/s12883-022-03046-w.
Broto A, Piñero-Lambea C, Segura-Morales C, Tio-Gillen A, Unger W, Burgos R, Mazzolini R, Verde S, Jacobs B, Huizinga R, Senar M, Serrano L. Engineering Mycoplasma pneumoniae to bypass the association with Guillain-Barré syndrome. Microbes Infect., 26(5-6), 105342 (2024) https://doi.org/10.1016/j.micinf.2024.105342.
Yao J, Zhou R, Liu Y, Lu Z. Progress in Guillain–Barré syndrome immunotherapy—A narrative review of new strategies in recent years. Hum Vaccin Immunother., 19(2), 2215153 (2023) https://doi.org/10.1080/21645515.2023.2215153.
Jain E, Pandav K, Regmi P, Michel G, Altshuler I. Facial diplegia: A rare, atypical variant of Guillain-Barré syndrome and Ad26.COV2.S vaccine. Cureus., 13(7), e16612 (2021) https://doi.org/10.1016/j.micinf.2024.105342.
Hull JH, Wootten M, Moghal M, Heron N, Martin R, Walsted E, Biswas A, Loosemolre M, Ellioot N, Ranson C. Clinical patterns, recovery time and prolonged impact of COVID-19 illness in international athletes: The UK experience. Br J Sports Med., 56(1), 4-11 (2022) https://doi.org/10.1136/bjsports-2021-104392.
Mahwish N, Omara EI, Rangraze IR, Al Qaeidy A. Post-bariatric Guillain-Barré syndrome: A case report emphasizing timely recognition and intervention. J Emerg Crit Care Med., 8, 2415 (2024) https://doi.org/10.21037/jeccm-23-142.
Zhang X, Yu D. Superacute onset of Guillain–Barré syndrome after elective spinal surgery: A case report and literature review. Medicine., 103(18), e37925 (2024) https://doi.org/10.1097/MD.0000000000037925.
Wen PY, Chen XW, Zhang M, Chu W, Hong-Liang W, Ren C. Guillain–Barre syndrome after myocardial infarction: A case report and literature review. BMC Cardiovasc Disord., 23(1), 226 (2023) https://doi.org/10.1097/MD.0000000000037925.
Altorfer FC, Weng A, Sneag DB, Pavlakis PP, Lebl DR. Guillain-Barré syndrome following lumbar spine surgery: A case report highlighting early magnetic resonance neurography findings. HSS J., 15563316241294049 (2024) https://doi.org/10.1177/15563316241294049.
Liu H, Shao S, Chen B, Yang S, Zhang X. Causal relationship between immune cells and Guillain-Barré syndrome: A Mendelian randomization study. Front Neurol., 15(2), 12567 (2024) https://doi.org/10.3389/fneur.2024.1446472.
Jahan I, Hayat S, Khalid MM, Ahammad A, Asad A, Islam B, Mohammad Q, Jacobs B, Islam Z. Association of mannose-binding lectin 2 gene polymorphisms with Guillain-Barré syndrome. Sci Rep., 12(1), 5791 (2022) https://doi.org/10.1038/s41598-022-09621-y.
Anilkumar AS, Veerabathiran R. The impact of Epstein-Barr virus on autoimmune neuromuscular disorders: A comparative study of myasthenia gravis and Guillain–Barre syndrome. Curr Treat Options Neurol., 26(11), 495-507 (2024) https://doi.org/10.1007/s11940-024-00809-3.
Zhai J, Yin Q, Dong S. Co-occurrence probability of typhoon surges affecting multiple estuaries in the northern coastal region of Taiwan. Reg Stud Mar Sci., 2(2), 101582 (2021) https://doi.org/10.1016/j.rsma.2020.101582.
Henny L, Thorncroft CD, Hsu HH, Bosart LF. Extreme rainfall in Taiwan: Seasonal statistics and trends. J Climate., 34(12), 4711-4731 (2021) https://doi.org/10.1175/JCLI-D-20-0999.1.
Liu TC, Wu TR, Hsu SK. Historical tsunamis of Taiwan in the 18th century: The 1781 Jiateng Harbor flooding and 1782 tsunami event. Nat Hazards Earth Syst Sci., 22(8), 2517-2530 (2022). https://doi.org/10.5194/nhess-22-2517-2022, 2022.
Yang S, Li S, Jin Y, Liu Z. Changing trends in cetacean strandings in the East China Sea: Identifying relevant variables and implications for conservation and management. Diversity., 15(10), 1082 (2023) https://doi.org/10.3390/d15101082.
Xu L, Zhao C, Bao Y, Liu Y, Liang Y, Wei J, Liu G, Wang J, Zhan S. Variation in worldwide incidence of Guillain-Barré syndrome: A population-based study in urban China and existing global evidence. Front Immunol., 15, 1415986 (2024) https://doi.org/10.3389/fimmu.2024.
Liu JJ, Xu Zhi, Xu Hui, Zhu J. Diagnostic status and epidemiological characteristics of community-acquired bacterial meningitis in children from 2019 to 2020: A multicenter retrospective study. BMC Pediatr., 24(1), 11 (2024) https://doi.org/10.1186/s12887-023-04469-1.
Phillips A, Jiang Y, Walsh D. Background rates of adverse events of special interest for COVID-19 vaccines: A multinational Global Vaccine Data Network (GVDN) analysis. Vaccine., 41(42), 6227-6238 (2023) https://doi.org/10.1016/j.vaccine.2023.08.079.
Li J, Shen L, Qian K. Global, regional, and national incidence and mortality of neonatal sepsis and other neonatal infections, 1990–2019. Front Public Health., 11, 8643 (2023) https://doi.org/10.3389/fpubh.2023.1139832.
Stoian A, Șerban G, Bajko Z, Andone S, Mosora O, Balasa A. Therapeutic plasma exchange as a first choice therapy for axonal Guillain Barré syndrome: A case based review of the literature. Exp Ther Med., 21, 1-12 (2021) https://doi.org/10.3892/etm.2021.9696.
Fernández-Fournier M, Kerguelen A, Rodriguez de Rivera FJ, Lacurez L, Jimeno S, Losantos I, Maraver D, Puertas I, Barranco A, Viejo A, Garcia A, Tejedor E. Therapeutic plasma exchange for myasthenia gravis, Guillain-Barre syndrome, and other immune-mediated neurological diseases, over a 40-year experience. Expert Rev Neurother., 22, 897-903 (2023) https://doi.org/10.1080/14737175.2022.2147827
Cekdemir D, Ozkan HA, Korkmaz F, Ozgurel Y, Kural S, Tiryaki N, Gulbas Z. Role of therapeutic plasma exchange in Guillain-Barre syndrome after allogeneic hematopoietic stem cell transplant: Report of two cases. Clin Lab., 67, 23678 (2021) https://doi.org/10.7754/Clin.Lab.2020.200613.
Li Y, Zhang X, Zhao C. Guillain‐Barre syndrome‐like polyneuropathy associated with immune checkpoint inhibitors: A systematic review of 33 cases. Biomed Res Int., 13, 4684 (2021) https://doi.org/10.1155/2021/9800488.
Chun JY, Park S, Jung J, Kim S, Choi Y, Kim H, Eom H, Hyun J. Guillain-Barré syndrome after vaccination against COVID-19. Lancet Neurol., 21, 117-119 (2022) https://doi.org/10.1016/S1474-4422(21)00416-6.
Kwan J, Biliciler S. Guillain-Barré syndrome and other acute polyneuropathies. Clin Geriatr Med., 37, 313-326 (2021) https://doi.org/10.1016/j.cger.2021.01.005.
Rosenthal A, Leviten M, Willison HJ, McGonigal R. Methods of treatment for Guillain-Barre syndrome. US Patent., 20160326237A1 (2016).
Adams C, Caffarelli MP, Ehara T, Karki RG, Mainolpi N. Piperidinyl indole derivatives and their use as complement factor b inhibitors. KR Patent., 102242742B1 (2021) https://doi.org/10.1007/s40262-022-01136-z.
Miller TA, Levenson JM, Martens L, Larson KC, Bruhn S. Shp1 and shp2 inhibitors and their methods of use. US Patent., 20220296616A1 (2022) https://doi.org/10.1177/11795735211057314.
Wang H. Glycan-based drugs, therapies and biomarkers. US Patent., 11285166B2 (2022).
O'Heeron P, Thomas I. Interaction of fibroblasts and immune cells and their use for activation. JP Patent., 7387603B2 (2023).
Leonhard SE, Tan CY, van der Eijk AA, Reisin RR, Franken SC, Huizinga R, Arends S, Batstra MR, Bezerra Jeronimo SM, Drenthen J, de Koning L, Leon Cejas L, Marchesoni C, Marques W Jr, Shahrizaila N, Casas DF, Sotelo A, Tillard B, Dourado ME, Jacobs BC. Antecedent infections in Guillain‐Barré syndrome in endemic areas of arbovirus transmission: A multinational case‐control study. J Peripher Nerv Syst., 26, 449-460 (2021) https://doi.org/10.1111/jns.12469.
Dutta D, Debnath M, Nagappa M, Das SK, Wahatule R, Sinha S, Taly AB, Ravi V. Antecedent infections in Guillain‐Barré syndrome patients from South India. J Peripher Nerv Syst., 26, 298-306 (2021) https://doi.org/10.1111/jns.12459.
Yıldırım M, Bektaş Ö, Botan E, Şahin S, Gurbanov A, Teber S, Kendirli T. Therapeutic plasma exchange in clinical pediatric neurology practice: Experience from a tertiary referral hospital. Clin Neurol Neurosurg., 207, 106823 (2021) https://doi.org/10.1016/j.clineuro.2021.106823.
Aslam N, Saleem S. Unravelling the antecedent symptoms in early presentation of Guillain-Barré syndrome: A comprehensive exploration. Pak J Physiol., 2, 36447 (2024) https://doi.org/10.69656/pjp.v20i2.1659.
Galassi G, Mazzoli M, Ariatti A, Bedin R, Marzullo D, Bastia E, Agnoletto V, Gozzi M, Valzania F, Meletti S, Marchioni A. Predictors of respiratory failure in Guillain-Barré syndrome: A 22 year cohort study from a single Italian centre. Eur J Neurol., 31, e16090 (2024) https://doi.org/10.1111/ene.16090.
Islam M, Ara A, Hasan S, Yusuf M, Karim R, Hoque M A, Mohammad Q D. Antecedent infections and hospital outcomes in demyelinating and axonal type of Guillain-Barre syndrome among adult patients. Bangladesh J Med Microbiol., 16, 19-24 (2022) https://doi.org/10.3329/bjmm.v16i1.65864.
Published
How to Cite
Issue
Section
Copyright (c) 2025 Sarika J Patil, Rohit R Bhosale, Dhanashri D Chavan, Akshay R Yadav, Swapnil S Patil

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
















